does medicaid cover tooth extraction?
Hi, welcome to solsarin site, in this post we want to talk about“does medicaid cover tooth extraction”,
stay with us.
does medicaid cover tooth extraction?
If they are deemed to be medically necessary, Medicaid will cover tooth extractions. A tooth extraction visit will consist of a $3.00 copay at the time of the visit.
Does Medicaid Cover Wisdom Teeth Removal for Adults?
Four sets of dual natures determine whether your Medicaid plan will cover wisdom teeth removal for adults in 2022.
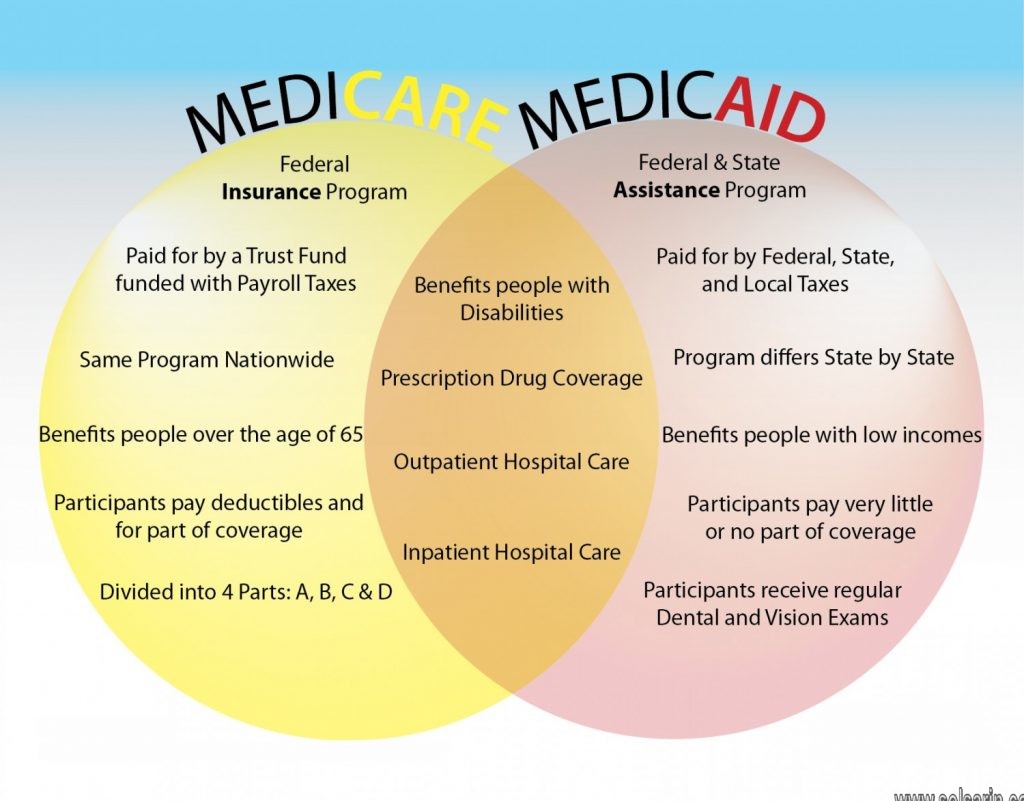
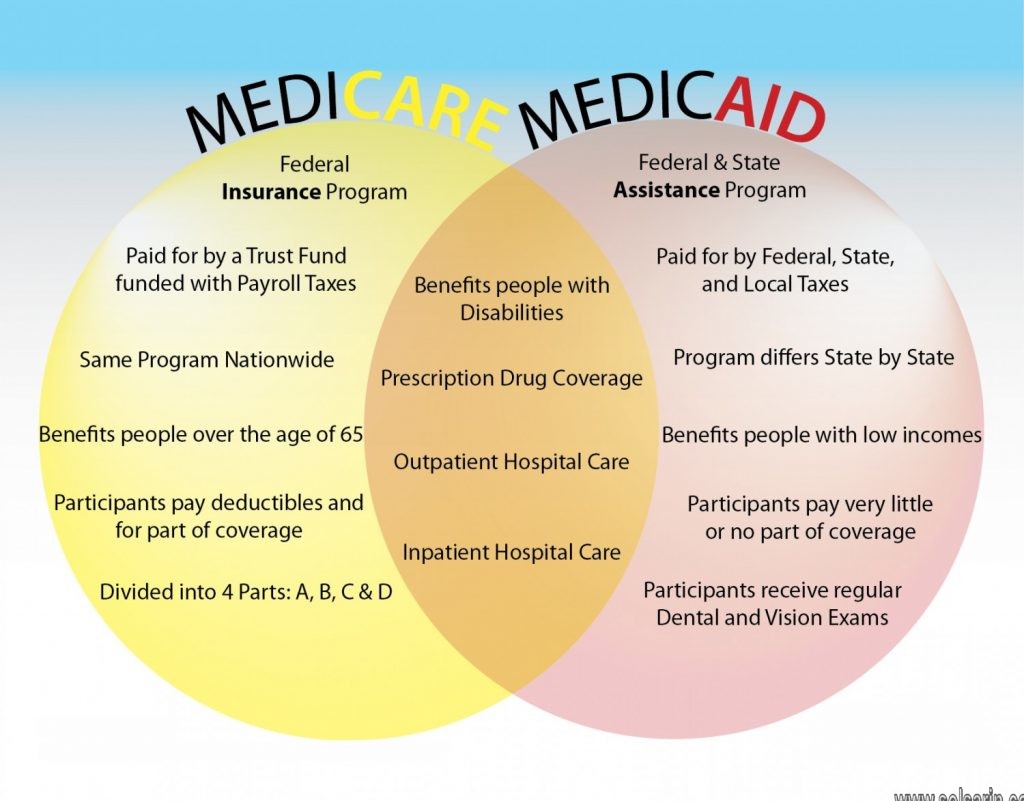
First, Medicaid is primarily health insurance with uniform rules across the country and dental insurance with uneven benefits in each state.
Second, oral and maxillofacial surgeons are medical doctors and dentists performing procedures billed to health and or dental insurance.
Third, the extraction of bony-impacted third molars fits under the health insurance component, and removing their gum-impacted counterparts falls into the dental insurance element.
Finally, the Managed Care Organization (bone-impacted) or Dental Benefits Manager (gum-impacted) adjudicates claims and is the final authority.
Does Medicaid cover dental care?
Dental services are a required service for most Medicaid-eligible individuals under the age of 21, as a required component of the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit.
Does Medicaid cover teeth whitening?
Medicaid does not cover teeth whitening, however, this service can still be paid for out of pocket at our office.
Does Medicaid Cover the Cost of Dental Care?
Each state has different qualifications and requirements that must be met for dental care to be covered by Medicaid. You will need to do some research to find out what the specific requirements are for your state.
About less than half the states will provide comprehensive dental benefits. On the other hand, in thirty-two states, Medicaid will cover dental care for certain categories, such as emergency dental services and medically necessary dental work.
Does Medicaid cover braces?
Medicaid may or may not cover braces. This is decided on a case by case basis, depending on what your dentist recommends, why you need braces, and location. If braces are needed to help with drastic problems in the patient’s mouth, they will likely be covered. Braces used for cosmetic reasons, however, will not be covered.
Medicaid Covers Bony-Impacted Wisdom Teeth Removal
The health insurance component of Medicaid should cover bony-impacted wisdom teeth removal, regardless of the state where you live. The rules apply uniformly nationwide when treating an illness, injury, disease, disability, or developmental condition.
Medically Necessary
Medicaid pays for the extraction of bony-impacted wisdom teeth when medically necessary under the health insurance component. Jawbone-impacted third molars fit this definition because they can cause pain and infection and develop cysts.
Oral and maxillofacial surgeons perform these complicated extractions, and your plan should pay for all costs associated with these medically necessary services.
- Extraction of partially or entirely bony third molars
- Therapeutic drug injection (Dexamethasone)
- Deep sedation (general anesthesia)
- Panoramic radiographic image
Finding a local oral surgeon who accepts Medicaid for bone-impacted wisdom teeth removal should prove relatively easy. They are licensed physicians whose offices regularly bill health insurance plans for services rendered.


Dental Benefits for Children in Medicaid
Medicaid covers dental services for all child enrollees as part of a comprehensive set of benefits, referred to as the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. Though oral screening may be part of a physical exam, it does not substitute for a dental examination performed by a dentist. A referral to a dentist is required for every child in accordance with the periodicity schedule set by a state.
Dental services for children must minimally include:
- Relief of pain and infections
- Restoration of teeth
- Maintenance of dental health
The EPSDT benefit requires that all services must be provided if determined medically necessary. States determine medical necessity. If a condition requiring treatment is discovered during a screening, the state must provide the necessary services to treat that condition, whether or not such services are included in a state’s Medicaid plan.
Each state is required to develop a dental periodicity schedule in consultation with recognized dental organizations involved in child health care. Dental services may not be limited to emergency services for children entitled to EPSDT.
Dental services must be provided at intervals that meet reasonable standards of dental practice, and at such other intervals, as indicated by medical necessity, to determine the existence of a suspected illness or condition. States must consult with recognized dental organizations involved in child health care to establish those intervals. A referral to a dentist is required for every child in accordance with each State’s periodicity schedule and at other intervals as medically necessary. The periodicity schedule for other EPSDT services may not govern the schedule for dental services.
Dental Services Covered by Medicaid
Children under 21 years of age enrolled in Medicaid receive a comprehensive set of benefits known as the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. At minimum, children must receive dental services that:
- Maintain dental health
- Restore teeth
- Relieve pain and infections
In addition, if a dental condition is uncovered through a regular dental examination and it requires treatment, the state must also provide the necessary treatment even if it isn’t normally part of what that state covers.
Here are examples of common dental services that might be provided include:
- Regular dental cleanings and exams
- Fluoride treatments
- Dental sealants
- Fillings
- Crowns
- Extractions
- Other dental services that are medically necessary (this includes emergency treatment as well)
If your child is covered by Medicaid, you will not need to pay co-payments or premiums for your child’s dental care. Our office is familiar with and will interact with the Medicaid office if there are any questions about our treatment plan. Find Medicaid and the Children’s Health Insurance Program (CHIP) coverage options for your family.


Adults Over 21
For adults over the age of 21, Medicaid will at least cover emergency and medically necessary dental work needed in almost all states. Sometimes Medicaid in specific states will opt to provide coverage in certain situations such as disabled adults who can’t provide for themselves, pregnant women, and low-income seniors.
However, there is no minimum requirement that Medicaid needs to meet for adult dental coverage.
Dental Benefits for Medicaid Adults
Dental treatment for adults is covered under certain circumstances through Virginia’s dental program, Smiles For Children.
Adult dental services are limited to medically necessary oral surgery and associated diagnostic services, such as X-rays and surgical extractions.
Preventive, restorative, endodontics, and prosthetic services (e.g. cleanings, fillings, root canals and dentures) are not covered for adults. Dental conditions that may qualify for reimbursement are ones compromising a patient’s general health and such conditions must be documented by the dentist or medical provider. Symptoms would include pain and/or infection.
Adult services require prepayment review by DentaQuest and providers have the option of requesting prior authorization.
Benefits Include
- Check-ups, x-rays, and cleanings every six months
- Tooth colored fillings for front teeth
- Silver fillings for back teeth
- Root canal treatment for certain teeth
- Removal of the soft inner part of the tooth (pulp) for infected baby teeth
- Pulling teeth
- Dentures, partial dentures
- Space maintainers for children with missing teeth
- Some orthodontic care for children
- Some specialty care for surgical centers for care under general anesthesia
- Emergency exams for acute onset of pain
- Crowns (porcelain and porcelain-to-metal crowns for certain populations)
does pregnancy medicaid cover tooth extraction?
Some people, who have many problems in their mouth and teeth, may have to undergo many dental procedures and may not be able to afford them. Many people, including pregnant women, with low income can enroll into Medicaid, depending on their state’s program (Galan 2018). Like other people, pregnant women still need to visit the dentist, and fortunately, they can utilize their Medicaid coverage for dental services.
Pregnant women need dental care, but they could postpone some procedures until they give birth to their baby. They should visit the dentist for “Preventive dental cleanings and annual exams” because “The rise in hormone levels during pregnancy causes the gums to swell, bleed, and trap food causing increased irritation to your [women’s] gums” (“Pregnancy And Dental Work” 2017). If these women do not receive preventive care, they can develop “oral infections such as gum disease, which has been linked to preterm birth” (“Pregnancy And Dental Work” 2017).
Pregnant women should also undergo other needed procedures, such as root canals and extractions in emergencies as well as cavity fillings and crowns “to reduce the chance of infection” (“Pregnancy And Dental Work” 2017). Usually, women in their second trimester can undergo dental procedures safely, but women in their third trimester may find “[lying] on your [their] back[s] [difficult] for an extended period of time” (“Pregnancy And Dental Work” 2017). Expectant women could schedule less urgent procedures, “such as teeth whitening and other cosmetic procedures… after the birth” since some procedures may endanger “the developing baby…” (“Pregnancy And Dental Work” 2017).
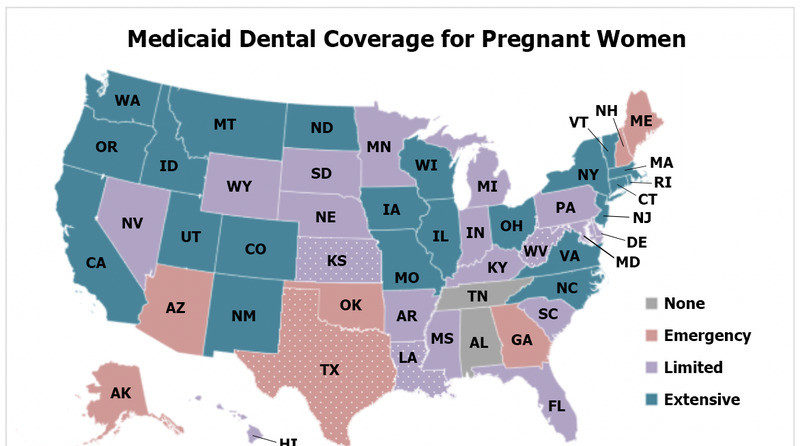
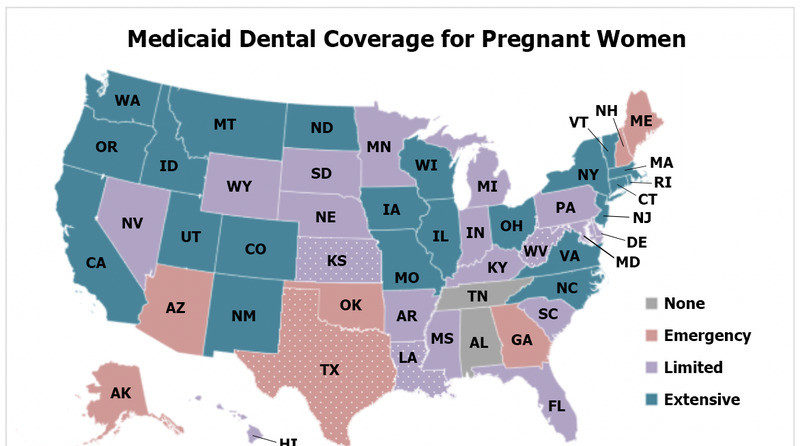
Medicaid Dental Coverage for Pregnant Women
With Medicaid, pregnant women with low income can pay for their dental care more easily. For pregnant “[w]omen under the age of 21,” the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit allows them to receive some coverage for “comprehensive dental care,” including “the relief of pain and infections, restoration of teeth, and maintenance of dental health” (Haney 2018; Haney 2017).
Meanwhile, those “over the age of 21” may receive dental coverage for certain procedures, depending on how their “state sets its own rules for the primary treatment categories,” which are emergency, preventive, restorative, periodontal, oral surgery, and orthodontia (Haney 2018; Haney 2017). For instance, in Louisiana, pregnant women can receive Medicaid coverage for procedures categorized under “Preventive, restorative, periodontal, and oral surgery,” while in Oklahoma, they can receive coverage for procedures categorized under “Preventive and restorative only” (Haney 2018).
Generally, states’ Medicaid programs usually cover fillings and root canals in order to “[stop] the spread of infections” and teeth cleanings to “[prevent] gum disease” (Haney 2018). While the states’ programs usually do not cover wisdom teeth extractions, they can cover pregnant women for these procedures in emergencies (Haney 2018).
Expectant women need to visit their dentists in order to take care of their teeth. For those with a tight budget, Medicaid coverage could alleviate the costs of their dental care.
MORE POSTS:




