Pathophysiology of myocardial infarction
Hello dear readers. In this post on Solsarin we are going to talk about ” Pathophysiology of myocardial infarction “. Continue reading to find the answer.please write your comment, Thank you for your attention.
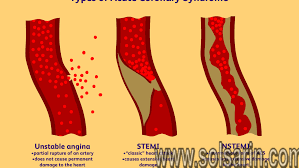
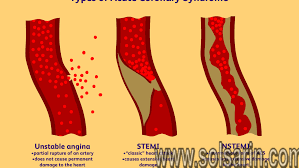
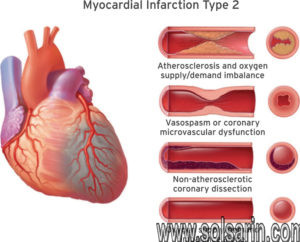
Myocardial infarction is a consequence of prolonged and severe imbalance between myocardial oxygen supply and demand. In the vast majority of cases, myocardial infarction results from coronary atherosclerosis with a superimposed luminal thrombus. Slowly developing high-grade coronary stenoses often progress to complete occlusion without causing acute myocardial infarction because formation of a collateral vascular network protects the cardiomyocytes from ischemic death. Myocardial infarction usually results from sudden occlusion of the coronary artery when a ‘high-risk’, thrombosis-prone plaque becomes eroded or ruptures.
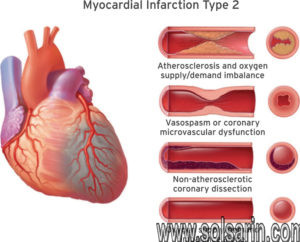
Stable angina, on the other hand, results from a myocardial oxygen delivery and demand mismatch in the setting of fixed coronary stenosis. After this discussion, the review article considers how both apply to perioperative myocardial infarctions and myocardial injury after noncardiac surgery.
This article furthermore argues why myocardial oxygen delivery demand mismatch (Type 2) myocardial infarction is the most likely underlying pathophysiology responsible for perioperative myocardial infarctions. Being aware of this and knowledgeable about Type 2 infarctions may enable anesthetic providers to better predict the majority of triggers contributing to, and thus decreasing the incidence of, perioperative myocardial infarctions.
Etiology
As stated above, myocardial infarction is closely associated with coronary artery disease. INTERHEART is an international multi-center case-control study which delineated the following modifiable risk factors for coronary artery disease:
-
Smoking
-
Abnormal lipid profile/blood apolipoprotein (raised ApoB/ApoA1)
-
Hypertension
-
Diabetes mellitus
-
Abdominal obesity (waist/hip ratio) (greater than 0.90 for males and greater than 0.85 for females)
-
Psychosocial factors such as depression, loss of the locus of control, global stress, financial stress, and life events including marital separation, job loss, and family conflicts
-
Lack of daily consumption of fruits or vegetables
-
Lack of physical activity
-
Alcohol consumption (weaker association, protective)
The INTERHEART study showed that all the above risk factors were significantly associated with acute myocardial infarction except for alcohol consumption, which showed a weaker association. Smoking and abnormal apolipoprotein ratio showed the strongest association with acute myocardial infarction. The increased risk associated with diabetes and hypertension were found to be higher in women, and the protective effect of exercise and alcohol was also found to be higher in women.
Other risk factors include a moderately high level of plasma homocysteine, which is an independent risk factor of MI. Elevated plasma homocysteine is potentially modifiable and can be treated with folic acid, vitamin B6, and vitamin B12.
Some non-modifiable risk factors for myocardial infarction include advanced age, male gender (males tend to have myocardial infarction earlier in life), genetics (there is an increased risk of MI if a first-degree relative has a history of cardiovascular events before the age of 50). The role of genetic loci that increase the risk for MI is under active investigation.
Epidemiology
The most common cause of death and disability in the western world and worldwide is coronary artery disease. Based on 2015 mortality data from the National Health Interview Survey (NHIS-CDC), MI mortality was 114,023, and MI any-mention mortality (i.e., MI is mentioned as a contributing factor in the death certificate) was 151,863.
As per the National Health and Nutrition Examination Survey (NHANES)-CDC data from 2011 to 2014, an estimated 16.5 million Americans older than 20 years of age have coronary artery disease, and the prevalence was higher in males than females for all ages. As per the NHANES 2011 through 2014, the overall prevalence of MI is 3.0% in US adults older than 20 years of age.
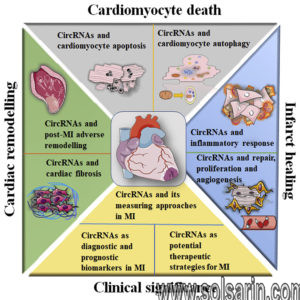
Pathophysiology
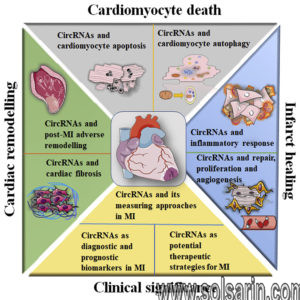
The acute occlusion of one or multiple large epicardial coronary arteries for more than 20 to 40 minutes can lead to acute myocardial infarction. The occlusion is usually thrombotic and due to the rupture of a plaque formed in the coronary arteries. The occlusion leads to a lack of oxygen in the myocardium, which results in sarcolemmal disruption and myofibril relaxation.These changes are one of the first ultrastructural changes in the process of MI, which are followed by mitochondrial alterations. The prolonged ischemia ultimately results in liquefactive necrosis of myocardial tissue. The necrosis spreads from sub-endocardium to sub-epicardium.
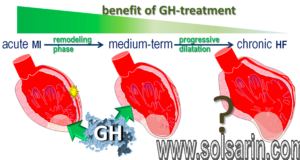
The subepicardium is believed to have increased collateral circulation, which delays its death. Depending on the territory affected by the infarction, the cardiac function is compromised. Due to the negligible regeneration capacity of the myocardium, the infarcted area heals by scar formation, and often, the heart is remodeled characterized by dilation, segmental hypertrophy of remaining viable tissue, and cardiac dysfunction.
History and Physical
The imbalance between oxygen supply and the demand leads to myocardial ischemia and can sometimes lead to myocardial infarction. The patient’s history, electrocardiographic findings, and elevated serum biomarkers help identify ischemic symptoms. Myocardial ischemia can present as chest pain, upper extremity pain, mandibular, or epigastric discomfort that occurs during exertion or at rest. Myocardial ischemia can also present as dyspnea or fatigue, which are known to be ischemic equivalents.
The chest pain is usually retrosternal and is sometimes described as the sensation of pressure or heaviness. The pain often radiates to the left shoulder, neck, or arms with no obvious precipitating factors, and it may be intermittent or persistent. The pain usually lasts for more than 20 minutes. It is usually not affected by positional changes or active movement of the region. Additional symptoms, such as sweating, nausea, abdominal pain, dyspnea, and syncope, may also be present. The MI can also present atypically with subtle findings such as palpitations, or more dramatic manifestations, such as cardiac arrest. The MI can sometimes present with no symptoms.
Prognosis
Within the first year after an MI, there is an additional mortality rate of 5% to 12%.Acute MI carries a mortality rate of 5-30%; the majority of deaths occur prior to arrival to the hospital.
- Overall prognosis depends on the extent of heart muscle damage and ejection fraction. Patients with preserved left ventricular function tend to have good outcomes.
Factors that worsen prognosis include:
- Diabetes
- Advanced age
- Delayed reperfusion
- Low ejection fraction
- Presence of congestive heart failure
- Elevations in C-reactive protein and B-type natriuretic peptide (BNP) levels
- Depression
Physical Therapy Management
Indications for Cardiac RehabCardiac Rehab is beneficial to patients of all ages who have had a heart attack, CAD, angina, or CHF. Other individuals who may gain benefits from this include post-surgical CABG, percutaneous intervention (PCI), or coronary angioplasty patients.
- A medical examination is completed at the initial consultation to determine the needs and limitations of the patient.
- The results of the exam are interpreted, the team creates a rehab program and sets goals for treatment.
- Treatment typically consists of a physical activity program in a group setting where vital signs can consistently be monitored. As the program progresses, the patient is taught how to monitor their own vitals and progresses to more challenging aerobic activities.
- Cycle Ergometer Use in the post-operative period following cardiac surgery is a safe choice for patient rehabilitation.
- Along with physical activity, patient education is also a very important part of cardiac rehab. Patients may work with a dietician or be given advice on how to stop smoking if necessary.
According to the American Heart Association, the benefits of cardiac rehab include:
- Regular physical activity helps your heart and the rest of your body get stronger and work better. Physical activity improves your energy level and lifts your spirits. It also reduces your chances of future heart problems, including heart attack.
- Counseling and education can help you quit smoking, eat right, lose weight, and lower your blood pressure and cholesterol levels. Counseling may also help you learn to manage stress and to feel better about your health.
- You have the advice and close supervision of healthcare professionals to help you improve your health and lower your risk of future problems. These professionals can also communicate with your primary care doctor or cardiologist.
Prevention
Evidence based interventions for secondary prevention include the use of aspirin, beta-blockers, angiotensin converting enzyme inhibitors; lipid lowering drugs and other anti- hypertensives, as well as modifying lifestyle related risk behaviours.
Physical exercise
Although the role of exercise alone in reducing cardiovascular outcomes is not clear, systematic reviews of RCTs have found that cardiac rehabilitation which includes physical exercise improves coronary risk factors and reduces the risk of major cardiac events in people after MI.
Dietary Modification
Stopping smokingRCTs have found that advising people with MI to eat more fish, fruit and vegetables, bread, pasta, potatoes, olive oil and margarine may result in a substantial survival advantage.
Apart from these pharmacological measures for secondary prevention, evidence is available that lifestyle measures such as stopping smoking, encouraging a healthy diet and exercise can also significantly contribute to reduction in cardiovascular mortality in people with established CVD.
Evidence from epidemiological studies indicates that people with coronary heart disease who stop smoking rapidly reduce their risk of recurrent coronary events or death. In the case of stroke survivors, observational studies have shown that the excess risk of stroke among former smokers largely disappeared 2-4 years after smoking cessation.
Medications
Following an MI, patients will most likely be prescribed some form of medication for the rest of their lives.
| Vasodilators (Nitrates) | Relaxes blood vessels and increases the supply of blood and oxygen to the heart while reducing its workload. Can come in pills to be swallowed, chewable tablets and as a topical application (cream). |
| Digitalis Preparations (Lanoxin) | Increases the force of the heart’s contractions, which can be beneficial in heart failure and for irregular heartbeats. |
| Statins | Various medications can lower blood cholesterol levels. They may be prescribed individually or in combination with other drugs. They work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood. |