treatment for plantar calcaneal enthesophyte
Hi everyone,This article on solsarin site is going to give you some information about”treatment for plantar calcaneal enthesophyte ”
Thank you for your considaration.
Definition/Description
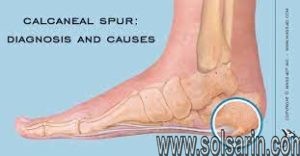
Heel spur
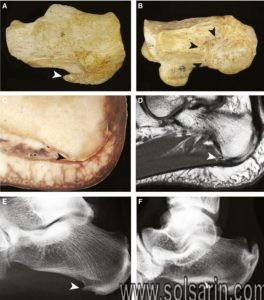
A calcaneal spur, or commonly known as a heel spur, occurs when a bony outgrowth forms on the heel bone. Calcaneal spurs can be located at the back of the heel (dorsal heel spur) or under the sole (plantar heel spur). The dorsal spurs are often associated with achilles Tendinopathy, while spurs under the sole are associated with Plantar fasciitis.
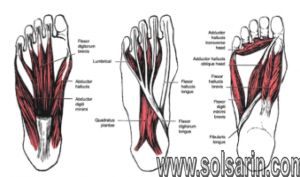
The apex of the spur lies either within the origin of the planter fascia (on the medial tubercle of the calcaneus) or superior to it (in the origin of the flexor digitorum brevis muscle). The relationship between spur formation, the medial tubercle of the calcaneus and intrinsic heel musculature results in a constant pulling effect on the plantar fascia resulting in an inflammatory response.
Clinically Relevant Anatomy
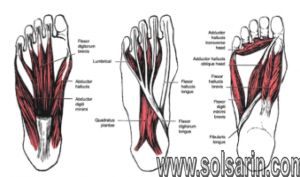
Intrinsic foot muscles
There are numerous muscles (Soleus, gastrocnemius, plantaris, abductor digiti minimi, flexor digitorum brevis, extensor digitorum brevis, abductor hallucis, extensor hallucis brevis, quadratus plantae) and the plantar fascia which exert a traction force on the tuberosity and adjacent regions of the calcaneus, especially when excessive or abnormal pronation occurs. The origin of the spurs appears to be caused by repetitive trauma which produces micro tears in the plantar fascia near its attachment and the attempted repair leads to inflammation which is responsible for the production and the maintenance of the symptoms.


Epidemiology /Etiology
The etiology of spurs has been debated. Heredity, metabolic disorders, tuberculosis, systemic inflammatory diseases and many other disorders have also been implicated. Current reasoning is that abnormal biomechanics (excessive or abnormal pronation) is the prime etiological factor for a painful plantar heel and inferior calcaneal spur. The spur is thought to be a result of the biomechanical fault and an incidental finding when associated with a painful plantar heel. The most common etiology is thought to be abnormal pronation which results in increased tension forces within the structures that attach in the region of the calcaneal tuberosity.
Asymptomatic heel spurs are relatively common in the normal, adult population. One epidemiologic study found that 11% of the adult U.S. population had developed a calcaneal spur which showed up on incidental radiographic finding.
Characteristics/Clinical Presentation
The painful heel is a relatively common foot problem, but calcaneal spurs are not considered as a primary cause of heel pain. A calcaneal spur is caused by long-term stress on the plantar fascia and foot muscles and may develop as a reaction to plantar fasciitis.
The pain, mostly localised in the area of the medial process of the calcaneal tuberosity, is caused by pressure in the region of the plantar aponeurosis attachment to the calcaneal bone. The condition may exist without producing symptoms, or it may become very painful, even disabling.
Most heel pain patients are middle-aged adults. Obesity may be considered a risk factor. Not all heel spurs cause symptoms and are often painless, but when they do cause symptoms people often experience more pain during weight-bearing activities, in the morning or after a period of rest. The pain, however, is not as a result of mechanical pressure on the spur, but from the inflammatory response.
There are 2 types of calcaneal spurs;
- Type A spurs are superior to the plantar fascia insertion
- Type B spurs extend forward from the plantar fascia insertion distally within the plantar fascia.
The mean spur length for type A is significantly longer statistically than the mean spur length for type B, although patients with type B spurs reported more severe clinical pain.
Spurs can be classified into 3 distinct types:
- There are those which are large in size, but which are asymptomatic, because the angle of growth is such that the spur aggravated through weight-bearing and/or the inflammatory changes have halted.
- The 2nd type are large, but painful on weight-bearing, because the pitch of the calcaneus has been changed by a depression of the longitudinal arch and, as a result, the spur may become a weight-bearing point, sometimes causing intractable refractory pain.
- This 3rd type has only a tiny amount of proliferation and its outline is irregular and jagged, usually accompanied by an area of decreased density around the origin of the plantar fascia, indicating a subacute inflammatory process. All calcaneal spurs undoubtedly begin in this manner, but only a few become symptomatic at this stage, because the etiologic factors are acute.
Differential Diagnosis
As chronic heel pain is a common manifestation of many conditions, these must be excluded before planning treatment. Diagnostic imaging as well as medical signs are often used to differentiate some of the conditions that are mentioned below from calcaneal spurs.
Musculoskeletal Causes
- Peroneal tendonitis: (inflammation of one or both peroneal tendons)
- MRI scan or ultrasound investigation
- Haglund’s deformity (with or without bursitis): symptomatic osseous posterior-superior prominence of the calcaneus
- Radiographs or Sonography of foot in maximal dorsiflexion
- Sever’s disease (calcaneal apophysitis): inflammation of the calcaneal apophysis due to overloading
- Clinical, Ultrasound investigations
Traumatic Influences
- Calcaneal fractures (and stress fractures): fractures as a consequence of repetitive load to the heel
- Ottawa Ankle Rules, Radiography, MRI (isotopic bone scan) and ultrasound.
Neurological Causes
- Baxter nerve entrapment: (chronic compression of the first branch of the lateral plantar nerve)
- Clinical (Tinel’s sign)
- Tarsal tunnel syndrome (sinus tarsi): Impingement of the posterior tibial nerve
- Clinical (Tinel’s sign, dorsiflexion-eversion test)
Other
- Heel fat pad syndrome: Atrophy or inflammation of the shock-absorbing fatty pad or corpus adiposum
- Clinical, ultrasound scan
- Chronic lateral ankle pain with other cause:
- MRI
Diagnostic Procedures
A diagnosis is based on the patient’s history and on the results of the physical examination. Diagnosis is usually confirmed by X-ray, but other diagnostic adjuncts are also used. Radiology may show calcaneal spur formation or calcification at either the insertion of the Achilles tendon or the origin of the plantar fascia. Rarely is an MRI required.
Outcome Measures
- Lower Extremity Functional Scale (LEFS)
- Outcome Measures Database
Examination
There are different aspects that need to be taken into consideration when performing the clinical examination.
- Is range of motion limited in the ankle and foot, especially passive dorsiflexion of the toes?
- Palpation of the proximal plantar fascia attachment at the heel. The presence of a calcaneal spur, any tenderness (site/severity) or deformities can be felt (in combination with the dorsiflexion)
- Is there any atrophy of the heel pad in comparison with the other foot in combination with reduced muscle strength?
- Is there any swelling?
- Sensation
- Presence of hypesthesias/dysthesias of the tibial nerve? Tinel’s sign
- Are there any skin tears on the foot?
- Any difference in foot alignment in comparison with the other foot?
- Aggravation on weight-bearing?
- Evaluation of gait
Management
‘The clinical practice guideline revision 2010 outlines different phases, divided in tiers. If a certain tier reduces symptoms, treatment should continue. If no improvement is reported, then treatment moves to a higher tier.
Recommended treatment timeline before moving up a tier if no improvement in symptoms:
Symptoms of Heel Spurs
Heel spurs often cause no symptoms. But heel spurs can be associated with intermittent or chronic pain — especially while walking, jogging, or running — if inflammation develops at the point of the spur formation. In general, the cause of the pain is not the heel spur itself but the soft-tissue injury associated with it.
Many people describe the pain of heel spurs and plantar fasciitis as a knife or pin sticking into the bottom of their feet when they first stand up in the morning — a pain that later turns into a dull ache. They often complain that the sharp pain returns after they stand up after sitting for a prolonged period of time.
Non-Surgical Treatments for Heel Spurs
The heel pain associated with heel spurs and plantar fasciitis may not respond well to rest. If you walk after a night’s sleep, the pain may feel worse as the plantar fascia suddenly elongates, which stretches and pulls on the heel. The pain often decreases the more you walk. But you may feel a recurrence of pain after either prolonged rest or extensive walking.
If you have heel pain that persists for more than one month, consult a health care provider. They may recommend conservative treatments such as:
- Stretching exercises
- Shoe recommendations
- Taping or strapping to rest stressed muscles and tendons
- Shoe inserts or orthotic devices
- Physical therapy
- Night splints
Heel pain may respond to treatment with over-the-counter medications such as acetaminophen (Tylenol), ibuprofen (Advil), or naproxen (Aleve). In many cases, a functional orthotic device can correct the causes of heel and arch pain such as biomechanical imbalances. In some cases, injection with a corticosteroid may be done to relieve inflammation in the area.


Surgery for Heel Spurs
More than 90 percent of people get better with nonsurgical treatments. If conservative treatment fails to treat symptoms of heel spurs after a period of 9 to 12 months, surgery may be necessary to relieve pain and restore mobility. Surgical techniques include:
- Release of the plantar fascia
- Removal of a spur
Pre-surgical tests or exams are required to identify optimal candidates, and it’s important to observe post-surgical recommendations concerning rest, ice, compression, elevation of the foot, and when to place weight on the operated foot. In some cases, it may be necessary for patients to use bandages, splints, casts, surgical shoes, crutches, or canes after surgery. Possible complications of heel surgery include nerve pain, recurrent heel pain, permanent numbness of the area, infection, and scarring. In addition, with plantar fascia release, there is risk of instability, foot cramps, stress fracture, and tendinitis.