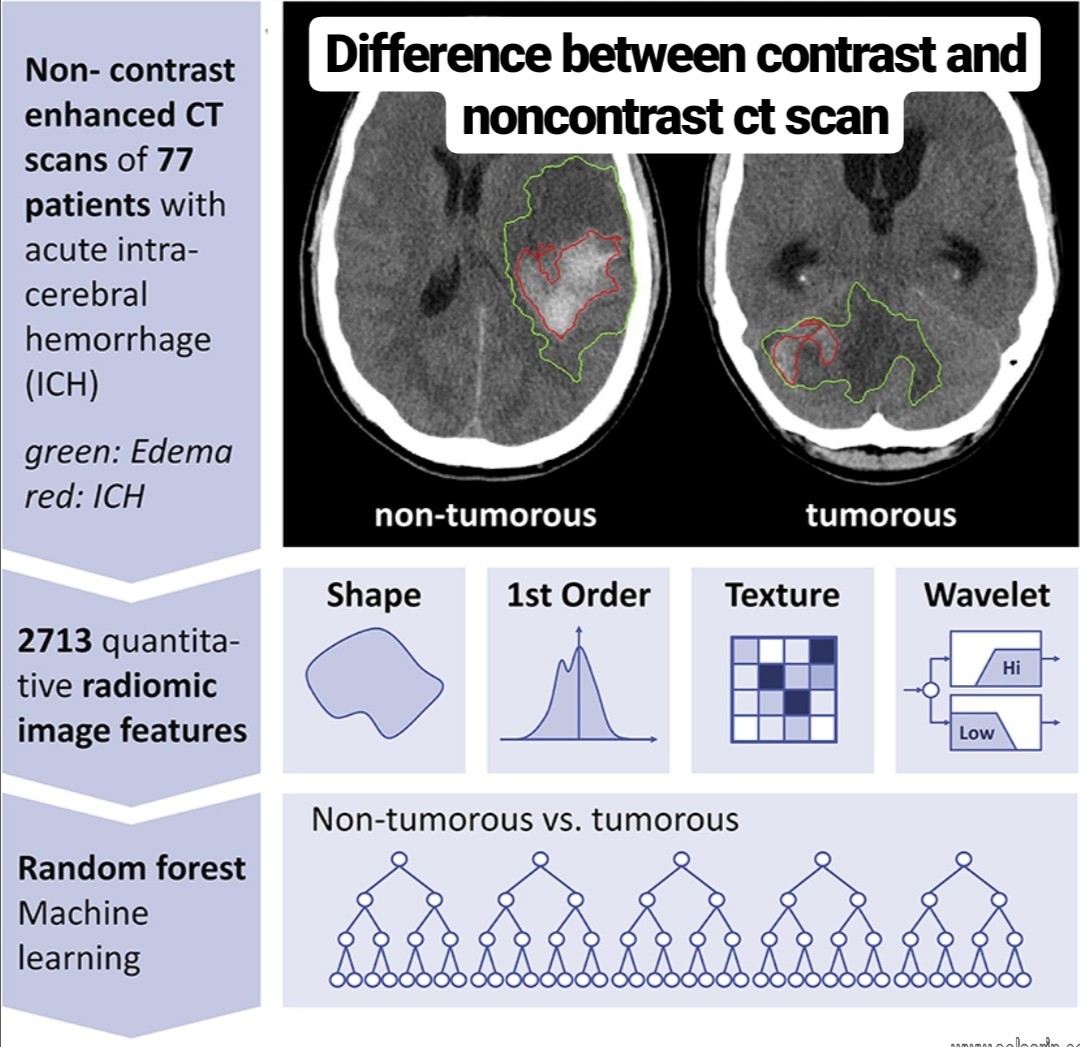
difference between contrast and noncontrast ct scan
Hi, welcome to solsarin site, in this post we want to talk about“difference between contrast and noncontrast ct scan”,
thank you for choosing us.
difference between contrast and noncontrast ct scan
| Area Of Body | Contrast CT Scan | Non-Contrast CT Scan |
|---|---|---|
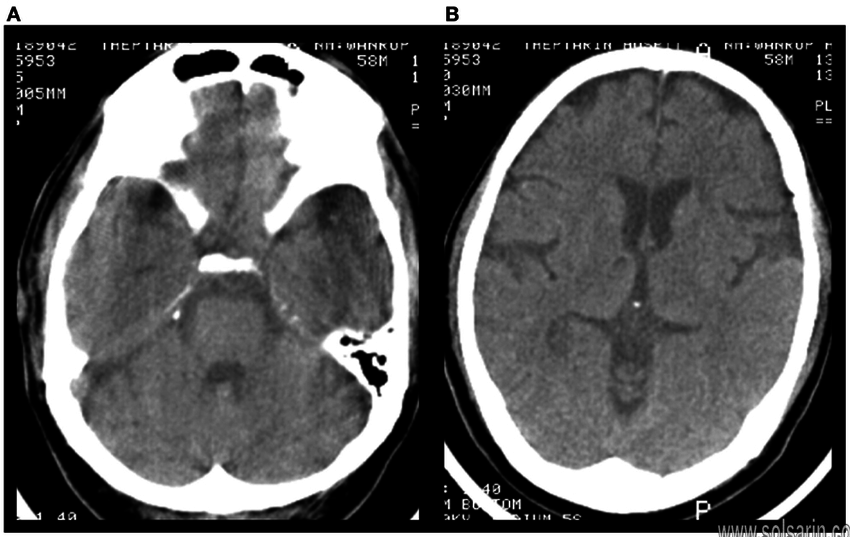
| Head CT Scan | Employed for meningeal enhancement, assessment of infection, abscess or tumor for example. Contrast-enhanced head CT is although much inferior to MRI for these indications and very less contrast-enhanced head CTs occur. | Used in case of stroke, headache, trauma and so on. Most things related to neurology use this technique. |
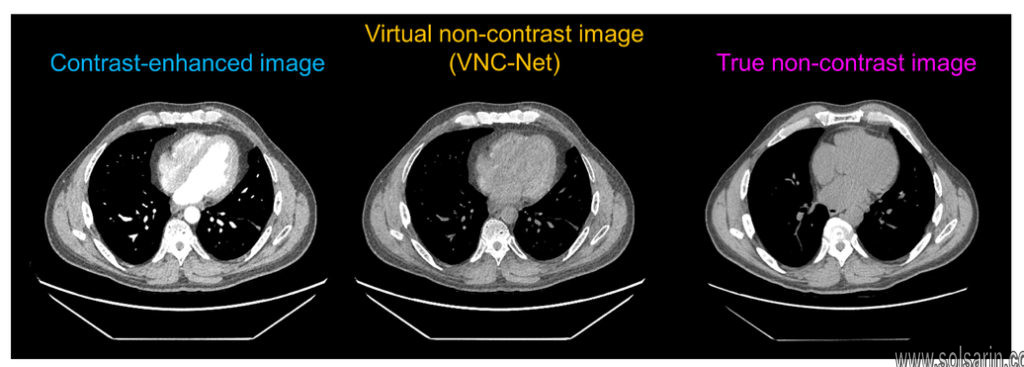
| Chest Computed Tomography (CT) | Employed for testing of the mediastinum (infections and lymph nodes). For evaluating the heart or vascular structures (CT Angiogram for things such as aneurysm, trauma, coronary CT). | Utilized for the purpose of Lung parenchymal evaluation, e.g. interstitial lung disease, lung nodules. |
| Abdomen/Pelvis Computed Tomography (CT) | Essentially everything else, like, Pancreatitis (essential), for the diffusion of abdominal pain, liver mass, abscess, diverticulitis, etc. | Used to find calculi in the ureters or kidneys (the other common sign is acute contrast allergy) Contrast-enhanced scans can make calculi unclear if the contrast begins to get discharged already. |
| CT Angiogram | Utilized for a few indications, like, Haematuria evaluation. Renal masses or abnormal growths in the kidney are found through contrast. | Only employed for a couple of purposes such as Haematuria evaluation. Non-contrast is utilized to find stones. |
Contrast or non-contrast study
Non-contrast studies of the brain and spine are sufficient for most indications. Diagnosis of common conditions such as cerebral infarction and haemorrhage can be made without intravenous contrast.
A contrast-enhanced CT of the brain is of value in specific situations (eg known CNS tumour, investigation for potential intracranial metastases, CNS infection). In addition, the imaging team may detect an unexpected abnormality on the plain scan at the time of scanning that warrants contrast administration.
CT neck and cerebral angiography is a specific contrast-enhanced technique that is valuable in the assessment of intracranial and neck vessels. The most common applications are in the assessment of patients with acute stroke who are potentially eligible for thrombolysis or mechanical clot retrieval, assessment of the extracranial carotid arteries in place of Doppler ultrasound or magnetic resonance angiography, and in subarachnoid haemorrhage.
Spinal CT imaging is usually performed without contrast. This is adequate for the assessment of fractures, degenerative disease, acute disc herniation, metastatic lesions, large epidural soft tissue lesions and established infection (eg discitis, osteomyelitis). Spinal cord detail is poor on CT; this is much better assessed with MRI.
What kinds of contrast are available?
- There are three broad kinds of contrast available: IV, PO, and PR (rectal). IV contrast is either gadolinium for MRI or iodinated contrast for CT. PO contrast for all ER and inpatient CT scans is dilute iodinated contrast (same agent used for IV contrast in CT). Barium is available as an alternative for ER patients with allergic reactions to iodinated contrast agents; currently the Department of Radiology recommends premedication for PO iodinated contrast in patients with a history of moderate or severe allergy (see departmental policy). Rectal contrast like oral contrast is dilute iodinated contrast, but administered through a rectal tube.
Types of Contrast Agents
The most common contrast agents used with CT imaging are barium- and iodine-based. The specific agent and route of administration are based on clinical indications and patient factors. Clear communication between the physician and radiologist is essential for obtaining the most appropriate study at the lowest cost and risk to the patient.
ORAL CONTRAST
The primary benefit of oral contrast is its ability to distend the bowels to help distinguish them from adjacent abdominal structures.
Oral contrast comes in two forms: neutral or positive. Neutral oral contrast consists of water or a dilute, low-attenuation solution that mirrors water. Positive oral contrast is an iodinated (ie, gastrografin) or barium-based solution with high attenuation that further demarcates bowel by opacification.
The advent of multidetector CT, which offers improved resolution, has made it easier to differentiate
abdominal structures without the need for the opacification with positive oral contrast. As a result,
some have argued that neutral oral contrast may be preferable to positive oral contrast due to similar efficacy, cost-effectiveness, and easier patient tolerability.
IV CONTRAST
Iodine-based intravenous (IV) contrast agents are used for opacification of vascular structures and solid abdominal and pelvic organs. The major families of contrast agents are ionic and nonionic. Contrast agents can be further classified as high or low osmolality, based on the iodine concentration. Most centers use nonionic contrast agents (which are generally low osmolality) for IV contrast studies.The rate of major reactions (e.g., anaphylaxis, death) is the same for ionic and nonionic IV contrast agents—an estimated one in 170,000 administrations—but nonionic contrast has a lower rate of minor reactions. Approximately 5% to 12% of patients who receive high-osmolality contrast have adverse reactions, most of which are mild or moderate. Use of low-osmolality contrast has been associated with a reduction in adverse effects. Children have a lower incidence of reactions to IV contrast agents, and most of these are mild (0.18% for low-osmolality agents).
Risk factors for contrast reactions include multiple drug allergies and asthma. Although many radiology departments screen for shellfish allergy, there is no cross-reactivity between shellfish and iodinated contrast. However, patients with a documented anaphylactic reaction to any medication are at higher risk of a reaction to iodinated contrast.
Many centers screen outpatients with suspected renal insufficiency by measuring serum creatinine one month before administration of contrast agents. Creatinine cutoffs vary among institutions, but generally range between 1.5 and 2 mg per dL (132.6 to 176.8 μmol per L) before alternative imaging strategies are considered. An increasing creatinine level that is still within normal limits is also concerning, and alternative imaging strategies should be considered. In patients with normal renal function, repeat measurement of serum creatinine is not recommended after outpatient administration of IV contrast agents.
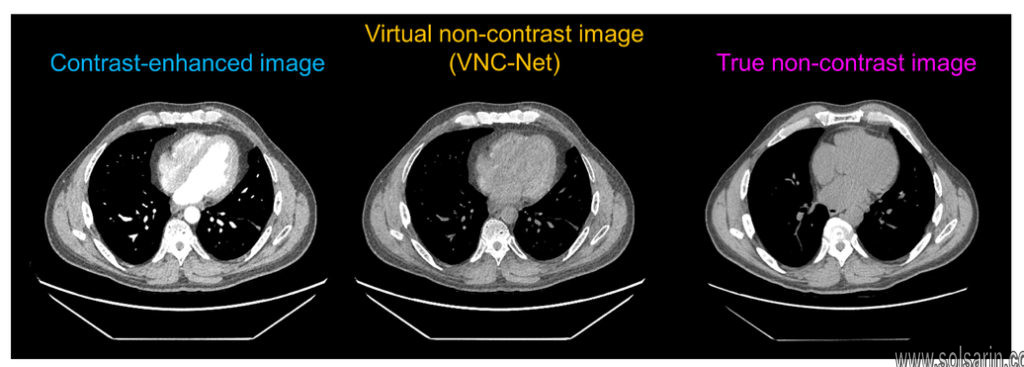
INTRAVENOUS CONTRAST
All modern IV contrast agents are iodine-based. The iodine causes increased absorption and scattering of the incoming radiation, which serves to increase the attenuation or “brightness” of the tissue or organ. Importantly, the IV contrast used in CT is distinct from the gadolinium-based IV contrast used in magnetic resonance imaging, meaning that there is no cross-reactivity between the two, which is important if the patient is allergic to one of them.
IV contrast is necessary for the evaluation of any kind of vascular disease, since it allows for easy identification of the blood vessel lumen. In abdominal imaging, IV contrast is recommended in most cases.


RECTAL CONTRAST
Rectal contrast can be used in patients with a suspected penetrating colonic injury.Rectal contrast does not always reach the cecum, so the small bowel and appendix can remain unopacified. Some centers use oral contrast to evaluate for appendicitis; some do not use bowel contrast, and others use rectal contrast to avoid the delay associated with oral administration.
What is a CT scan of the abdomen?
Computed tomography (CT scan or CAT scan) is a noninvasive diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, organs, and blood vessels. CT scans are more detailed than standard X-rays.
In standard X-rays, a beam of energy is aimed at the body part being studied. A plate behind the body part captures the variations of the energy beam after it passes through skin, bone, muscle, and other tissue. While much information can be obtained from a standard X-ray, a lot of detail about internal organs and other structures is not available.
In computed tomography, the X-ray beam moves in a circle around the body. This allows many different views of the same organ or structure.Moreover, The X-ray information is sent to a computer that interprets the X-ray data and displays it in a two-dimensional (2D) form on a monitor.
What is a CT scan of the abdomen?
CT scans may be done with or without “contrast.” Contrast refers to a substance taken by mouth or injected into an intravenous (IV) line that causes the particular organ or tissue under study to be seen more clearly. Contrast examinations may require you to fast for a certain period of time before the procedure. Your doctor will notify you of this prior to the procedure.
So, CT scans of the abdomen can provide more detailed information about abdominal organs and structures than standard X-rays of the abdomen, thus providing more information related to injuries and/or diseases of the abdominal organs.
CT scans of the abdomen may also be used to visualize placement of needles during biopsies of abdominal organs or tumors or during aspiration (withdrawal) of fluid from the abdomen. CT scans of the abdomen are useful in monitoring tumors and other conditions of the abdomen before and after treatment.
Other related procedures that may be used to diagnose abdominal problems include abdominal X-rays, pancreas scan, liver scan, gallbladder scan, kidney scan, endoscopy procedures such as colonoscopy, abdominal ultrasound, and abdominal angiogram.
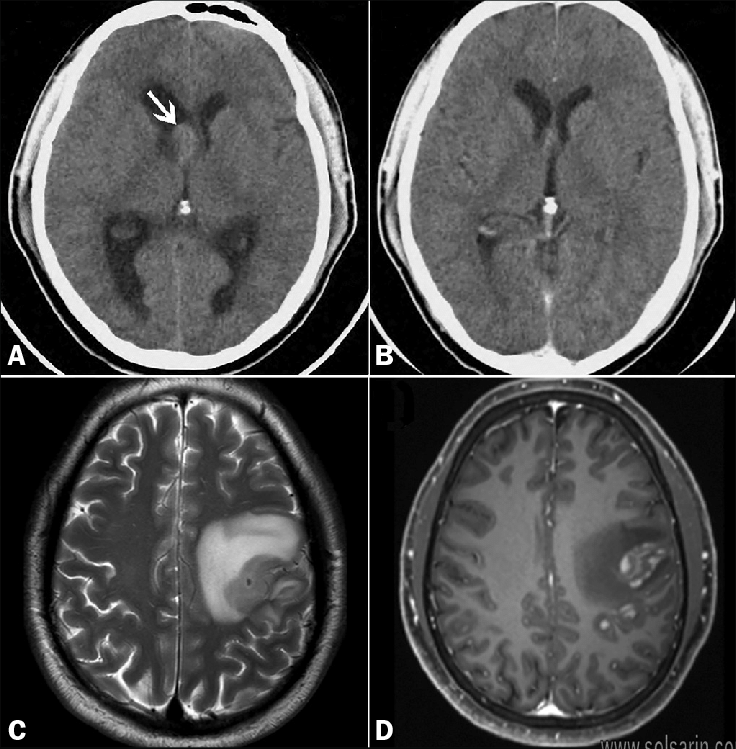
MRI Contrast vs. Non-contrast
There are two major types of MRI scans; contrast and non-contrast. When a patient is undergoing a contrast MRI, a dye that is gadolinium-based is given to the patient intravenously. A contrast agent will only be used when ordered by a physician, allowing the radiologist to more accurately report on
how the patient’s body is working and whether any disease or abnormality is present. The gadolinium contrast medium enhances and improves the quality and clarity of the MRI images.
However, in most cases a non-contrast MRI is an effective exam for imaging the body’s organs. Even without the intravenous contrast, MRI can detect pathology in most organs and in some cases the
pathology is made less visible on a contrast MRI than a non-contrast scan. For example, non-contrast scans provide greater images of blood vessel activity to detect aneurysms and blocked blood vessels.1 The results of an MRI procedure without contrast are just as valuable and relevant as those done with the use of a contrast agent.
MRI contrast is required when a very detailed image is necessary to evaluate the problem area of the body. Moreover, Gadolinium contrast is used in about one in three MRI scans, to improve the diagnostic accuracy of the scan.Moreover, Adding contrast to the image enhances the visibility of inflammation, tumors, blood vessels and the blood supply of certain organs. The decision of whether to use contrast during
a scan depends on the type of problem and the health history of the patient.
The three main differences between a contrast and non-contrast scan are:
- Typically, if an MRI procedure is done with a contrast agent then there will be no need for additional MRI procedures due to the high resolution of the resulting image. A non-contrast scan may require additional procedures to clarify any abnormalities.
- MRI with contrast is superior at measuring and assessing tumors. Contrast helps detect even
the smallest tumors, giving the surgeon more clarity regarding the location and size of the tumor and other tissues involved.
- MRI images with contrast are clearer and better quality than the images without contrast.