principal diagnosis definition
Hi, welcome to solsarin site, in this post we want to talk about“principal diagnosis definition”,
stay with us.
principal diagnosis definition
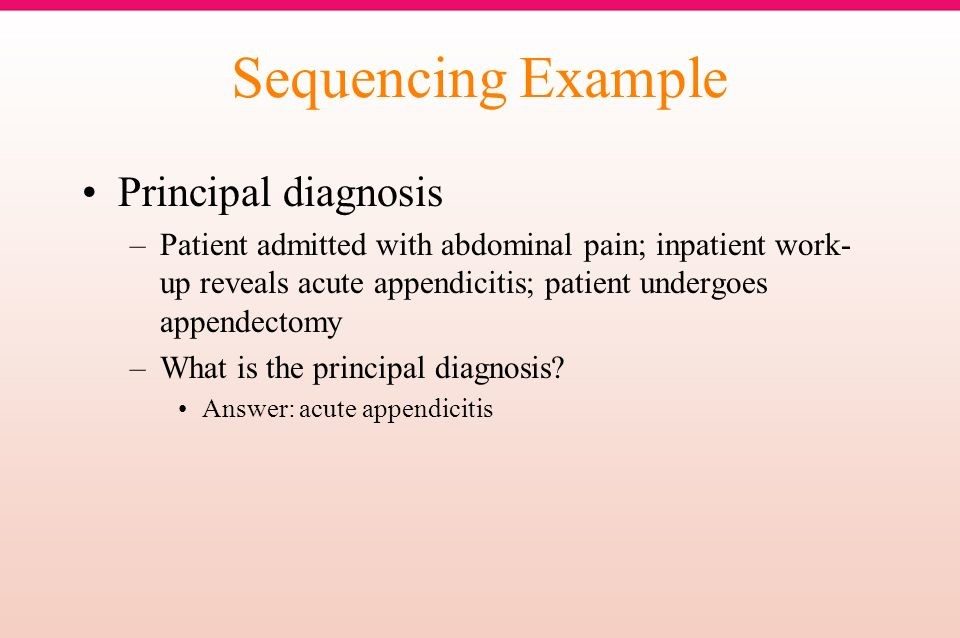
The principal diagnosis is defined as the “condition, after study, which caused the admission to the hospital,”
according to the ICD-10-CM Official Guidelines for Coding and Reporting, FY 2016. This is not necessarily what brought the patient to the emergency room.
For example: A patient is admitted for a total knee replacement for osteoarthritis. The patient is
brought to the preoperative holding area to prepare for surgery and suffers a ST-segment elevation
myocardial infarction (STEMI) before the surgery can begin. Instead of going to the operating room for the knee replacement, the patient goes to the cath lab for a stent placement.
The principal diagnosis in this instance is the osteoarthritis. Acute myocardial infarction (the STEMI) is not the principal diagnosis because it was not the condition that caused the admission. It is the secondary diagnosis.
What is a principal diagnosis?
Principal diagnosis describes the underlying cause behind a patient’s initial hospital admission and is assigned only after a physician has completed necessary tests and examinations. This is distinct from an admitting diagnosis—which describes a patient’s condition at the time of hospital admission before formal tests have been administered.
Occasionally, complications and comorbidities may overtake the principal diagnosis in terms of treatment length and aggressiveness. In this case, the more resource-intensive condition is called the primary diagnosis.
Definition of Principal Diagnosis in the Official Guidelines
As all of you are aware, we continue to struggle with the definition of “principal diagnosis” for residents who remain in the nursing home. The Coding Team of the LTC Practice Council recently asked Sue Bowman, RHIA, CCS, AHIMA’s director of coding policy and compliance, for her opinion on whether the guidance in Coding Clinic Fourth Quarter 1999 related to “continued stay” in the nursing home could be added as a “note” in the official guidelines (Section II, Definition of Principal Diagnosis). In this 1999 Coding Clinic, the Cooperating Parties, in conjunction with the Editorial Advisory Board of Coding Clinic, indicated the following:
The “first listed diagnosis” is the diagnosis that is chiefly responsible for the admission to, or continued residence in, the nursing facility and should be sequenced first. For example, when coding an admission to the facility, the “first listed diagnosis” is the condition chiefly responsible for the admission to the facility. If coding diagnoses during the resident’s stay, it is the condition chiefly responsible for the continued stay in the facility.
Definition of Principal Diagnosis in the Official Guidelines
Bowman’s response indicated that the Coordination and Maintenance Committee does not address data set definition issues; it only addresses modifications to the ICD-9-CM coding system. The coding guidelines merely represent the definitions that are in the Uniform Hospital Discharge Data Set (UHDDS), which are part of the data standards for the data elements on the UB-04.
As noted in the definition of principal diagnosis, this definition was published in the Federal Register in 1985. The use of this definition was extended to include all providers using the UB-04 billing form (or its electronic counterpart, the 4010) and expect these providers to use the UHDDS definition for reporting the principal diagnosis. Since the cooperating parties do not “define” data definitions, they are not able to include the expansion for “continued stay” in the regulatory definition.


Definition
The Principal/Primary Diagnosis is the condition established after study to be chiefly responsible for
occasioning the admission of the patient to the hospital for care. Since the Principal/Primary Diagnosis represents the reason for the patient’s stay, it may not necessarily be the diagnosis which represents the greatest length of stay,
the greatest consumption of hospital resources, or the most life-threatening condition. Since the
Principal/Primary Diagnosis reflects clinical findings discovered during the patient’s stay, it may differ from Admitting Diagnosis.
In the case of admission to the hospital-based ambulatory surgery service or freestanding ambulatory surgery center,
the Principal/Primary Diagnosis is that diagnosis established to be chiefly responsible for occasioning the admission to the service or center for the specific procedure.
In the case of emergency department visits, the Principal/Primary Diagnosis Code is that diagnosis established to be chiefly responsible for occasioning the visit to the Emergency Department.
Two or more possible principal diagnoses
In some cases, two conditions could be equally responsible for the admission. ICD-9-CM Official Guidelines for Coding and Reporting specifically address this possibility. Section II.c states:
In the unusual instance when two or more diagnoses equally meet the criteria for principal diagnosis as determined by the circumstances of admission, diagnostic workup and/or therapy provided,
and the Alphabetic Index, Tabular List, or another coding guidelines does not provide sequencing direction, any one of the diagnoses may be sequenced first.
Consider a patient who is admitted for acute respiratory failure due to exacerbation of congestive heart failure (CHF).
Either condition could be the principal diagnosis,
says Cheryl Ericson, MS, RN, CCDS, CDIP, CDI education director for HCPro, a division of BLR in Danvers, Massachusetts. When a patient is admitted with acute respiratory failure and another
condition, coders and CDI specialists don’t always agree on the principal diagnosis.
Many coders view these diagnoses as equal and apply the coding guideline regarding two diagnoses
that equally meet the definition of the principal diagnosis. The CDI specialist may consider acute respiratory failure as the principal diagnosis, leading to one MS-DRG,
while the coder uses congestive heart failure as the principal diagnosis, resulting in a different MS-DRG assignment.


Codes
As I respond to coding questions and review records,
the one key factor that continues in every chart whether inpatient, outpatient, emergency,
or ancillary is principal diagnosis or first-listed condition. In order to ensure “reason for admission
after study”, medical necessity, and reason for the encounter is accurately reflected, we look first to the Uniform Discharge Data Set (UHDDS) guidelines.
- Principal Diagnosis (PDX): The circumstances of inpatient admission always govern the selection of the principal diagnosis. Coding directives in the ICD-10 CM classification take precedence over all other guidelines. “…that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care.”
- Admission follow Medical Observation/Post- Operative Observation: Report the medical condition that led to the hospital admission, which may be different from the reason the patient was admitted to observation.
- Admission from Out- patient Surgery: If the reason for the inpatient admission is another condition unrelated to the surgery, assign the unrelated condition as the principal diagnosis. If the reason is a complication, assign the complication as the principal diagnosis.
- Abnormal Findings: When findings are clearly outside the normal range and the physician has ordered other tests to evaluate the condition or has prescribed treatment without documenting an associated diagnosis, it is appropriate to ask the physician whether a diagnosis should be added or whether the abnormal finding should be listed in the diagnostic statement. Incidental findings on X-rays should not be reported unless further evaluation or treatment is carried out.
Why is a principal diagnosis an important metric in healthcare?
Principal diagnosis serves an important function in determining which diagnosis-related group (DRG) code to assign a patient. DRGs and other diagnostic codes, like ICD-10, are not only used to electronically record a patient’s treatment history, but they also play a crucial role in healthcare billing.
Healthcare providers will use these codes to determine the complexity of patient treatment. This includes the symptoms they initially presented and the medications, treatments, procedures, and other hospital resources that they received. This information helps care providers know how to bill an insurer for a given episode of care.
No established diagnosis
Several guidelines identify the appropriate reporting when the physician has not established a definitive diagnosis. If the physician’s diagnostic statement identifies a symptom followed by contrasting/comparative diagnoses,
the ICD-9-CM Official Guidelines for Coding and Reporting instruct coders to sequence the symptom first (principal diagnosis) and report the contrasting/comparative diagnoses as additional diagnoses.
For example, if the physician’s diagnostic statement said chest pain,
coronary artery disease (CAD) vs. pneumonia, then chest pain would be the principal diagnosis based on the coding guideline, Avery says.
However, if the physician simply lists two or more contrasting/comparative diagnoses then either can be sequenced first. So if the physician simply wrote CAD vs. pneumonia, then either could be sequenced as principal diagnosis, Avery says. The coder should use the circumstances of the
admission, therapy provided, etc., to make the determination if one outweighs the other.
Elements of a diagnosis
The DSM 5 states that the following make up the key elements of a diagnosis (APA, 2013):
Diagnostic Criteria and Descriptors
Diagnostic criteria are the guidelines for making a diagnosis. When the full criteria are met, mental health professionals can add severity and course specifiers to indicate the patient’s current presentation. If the full criteria are not met, designators such as “other specified” or “unspecified” can be used. If applicable, an indication of severity (mild, moderate, severe, or extreme), descriptive features, and course (type of remission – partial or full – or recurrent) can be provided with the diagnosis. The final diagnosis is based on the clinical interview, text descriptions, criteria, and clinical judgment.
Subtypes and Specifiers
Subtypes denote “mutually exclusive and jointly exhaustive phenomenological subgroupings within a diagnosis” (APA, 2013). For example, non-rapid eye movement sleep arousal disorders can have either a sleep walking or sleep terror type. Enuresis is nocturnal only, diurnal only, or both. Specifiers are not mutually exclusive or jointly exhaustive and so more than one specifier can be given. For instance, binge eating disorder has remission and severity specifiers. Somatic symptom disorder has a specifier for severity, if with predominant pain, and/or if persistent. Again the fundamental distinction between subtypes and specifiers is that there can be only one subtype but multiple specifiers.
Principle Diagnosis
A principal diagnosis is used when more than one diagnosis is given for an individual. It is the reason for the admission in an inpatient setting, or the reason for a visit resulting in ambulatory care medical services in outpatient settings. The principal diagnosis is generally the main focus of treatment.
Provisional Diagnosis
If not enough information is available for a mental health professional to make a definitive diagnosis, but there is a strong presumption that the full criteria will be met with additional information or time, then the provisional specifier can be used.
MORE POSTS: